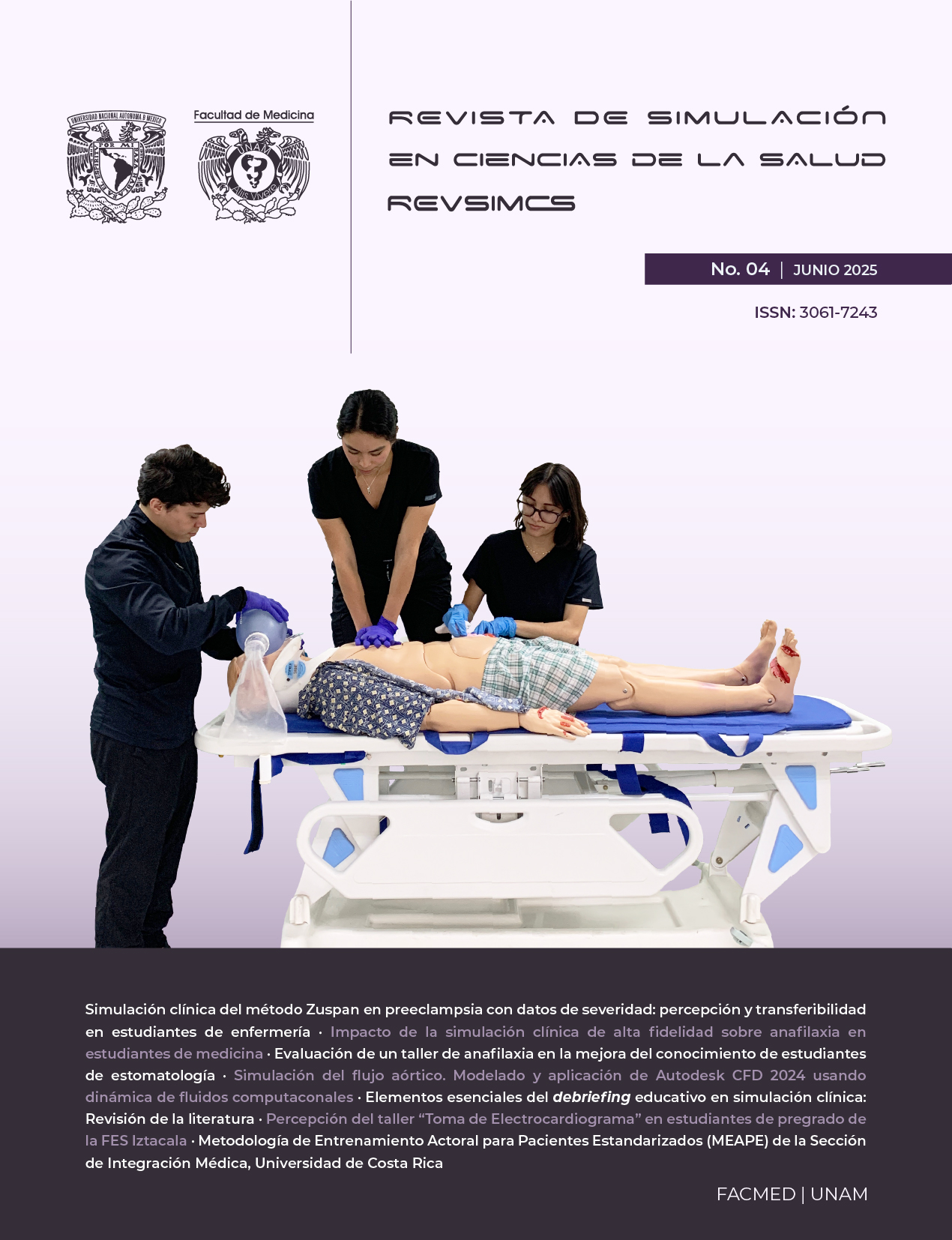
Acting Training Methodology for Standardized Patients (MEAPE) of the Medical Integration Section, University of Costa Rica
DOI:
https://doi.org/10.22201/fm.30617243e.2025.4.112Keywords:
Patient Simulation, Science in the Arts, Medical Education, Interdisciplinary ResearchAbstract
This methodological proposal emerges from an action-research process by the Drama Arts team of the Medical Integration Section (SIM) at the University of Costa Rica, aiming to document a comprehensive actor training model for Standardized Patients (SPs) in clinical simulation. The MEAPE methodology is based on theatrical realism, particularly Stanislavski's Method of Physical Actions and Meisner's moment-to-moment work, adapted to medical education. It consists of five phases: clinical script analysis, character construction, rehearsal, scenario simulation, and feedback (debriefing), including a critical self-assessment stage. The model emphasizes three-dimensional characters with biopsychosocial coherence, enhancing realistic, empathetic learning experiences. Collaboration between medical and drama professionals aligns pedagogical and performative goals, optimizing fidelity and educational impact.
References
A Benedetti, J. (2005). Stanislavski y el trabajo del actor (5.ª ed.), Alba Editorial.
Cleland, J. A., Abe, K., & Rethans, J. J. (2009). The use of simulated patients in medical education: AMEE Guide No 42. Medical Teacher, 31(6), 477–486. https://doi.org/10.1080/01421590903002821
Dawson, R. M., Lawrence, K., Gibbs, S., Davis, V., Mele, C., & Murillo, C. (2021). “I Felt The Connection”: A Qualitative Exploration of Standardized Patients’ Experiences in a Delivering Bad News Scenario. Clinical Simulation in Nursing, 55, 52–58. https://doi.org/10.1016/j.ecns.2021.04.012
Gaba, D. M. (2004). The future vision of simulation in health care. Quality and Safety in Health Care, 13(suppl 1), i2–i10. https://doi.org/10.1136/qhc.13.suppl_1.i2
Gliva-McConvey, G. (2020). Standardized patient methodology in health professions education. In K. T. Bosse (Ed.), Clinical simulation: Education, operations, and engineering (pp.183–200). Elsevier.
INACSL Standards Committee. (2021). Healthcare Simulation Standards of Best Practice™: Prebriefing: Preparation and briefing. Clinical Simulation in Nursing, 58, 9–13. https://doi.org/10.1016/j.ecns.2021.08.008
Kol, E., Ince, S., Işik, R. D., Ilaslan, E., & Mamakli, S. (2021). The effect of using standardized patients in the Simulated Hospital Environment on first-year nursing students psychomotor skills learning. Nurse Education Today, 107, 105147. https://doi.org/10.1016/j.nedt.2021.105147
Kucukkelepce, G. E., Dinc, L., & Elcin, M. (2021). Views of nursing students on using standardized patient and in-class case analysis in ethics education. Nurse Education Today, 107, 105155. https://doi.org/10.1016/j.nedt.2021.105155
Lewis, K., Bohnert, C., Gammon, W., Hölzer, H., Lyman, L., Smith, C., Thompson, T., Wallace, A., & Gliva-McConvey, G. (2017). The Association of Standardized Patient Educators (ASPE) Standards of Best Practice (SOBP). Advances in Simulation, 2(10). https://doi.org/10.1186/s41077-017-0043-4
May, W., Park, J. H., & Lee, J. P. (2009). A ten-year review of the literature on the use of standardized patients in teaching and learning: 1996–2005. Medical Teacher, 31(6), 487–492. https://doi.org/10.1080/01421590802530898
Meisner, S., & Longwell, D. (1987). Sanford Meisner on acting. Vintage Books.
Moore, P. M., Rivera Mercado, S., Grez Artigues, M., & Lawrie, T. A. (2018). Communication skills training for healthcare professionals working with people who have cancer. Cochrane Database of Systematic Reviews, (7). https://doi.org/10.1002/14651858.CD003751.pub4
Motola, I., Devine, L. A., Chung, H. S., Sullivan, J. E., & Issenberg, S. B. (2013). Simulation in healthcare education: A best evidence practical guide. AMEE Guide No. 82. Medical Teacher, 35(10), e1511–e1530. https://doi.org/10.3109/0142159X.2013.818632
Nestel, D., & Tierney, T. (2007). Role-play for medical students learning about communication: Guidelines for maximising benefits. BMC Medical Education, 7, 3. https://doi.org/10.1186/1472-6920-7-3
Reinhardt, A. C., León, T. G., DeBlieck, C., & Amatya, A. (2019). Using simulations to advance clinical reasoning. Applied Nursing Research, 47, 63-70. https://doi.org/10.1016/j.apnr.2019.05.005
Rudolph, J. W., Simon, R., Dufresne, R. L., & Raemer, D. B. (2006). There’s no such thing as “nonjudgmental” debriefing: A theory and method for debriefing with good judgment. Simulation in Healthcare, 1(1), 49–55. https://doi.org/10.1097/01266021-200600110-00006
Society for Simulation in Healthcare. (2020). Definition of healthcare simulation. https://ssih.org/sites/default/files/2025-03/Healthcare-Simulation-Dictionary-3.pdf
Stanislavski, K. (2013). An Actor Prepares (E. R. Hapgood, Trans.). Bloomsbury Publishing.
Talente, G., Haist, S. A., & Wilson, J. F. (2003). A model for setting performance standards for standardized patient examinations. Evaluation & the Health Professions, 26(4), 427–446. https://doi.org/10.1177/0163278703258105
Yudkowsky, R., Park, Y. S., & Downing, S. M. (2022). Assessment in health professions education (2nd ed.). Routledge. https://www.taylorfrancis.com/books/edit/10.4324/9781138054394/assessment-health-professions-education-rachel-yudkowsky-yoon-soo-park-steven-downing